- Home
- David Fajgenbaum
Chasing My Cure Page 16
Chasing My Cure Read online
Page 16
It wasn’t a deep mystery why.
I was proud: I just didn’t want to be treated differently. I didn’t want to be that “sick guy.” Like the kid at summer camp with the asthma inhaler whom the counselors always kept on the sidelines. Only in this case, with a disease that none of them would recognize or understand—after all, the medical community barely understood it. My med school friends knew me before I was sick, and they stuck with me afterward. But I had never made new friends as the sick guy. Before I got sick, I was always the helper, the supporter. I liked that role; it’s something I clearly inherited from my mom. I didn’t like being the one in need of help. I realized I was experiencing something that many of my patients had known intimately. It’s different being sick, apart from the vagaries of the actual sickness. It makes you different. In ways that can very quickly feel unfair.
I was afraid: There really were vulnerabilities to my being sick. As I’d discovered at the medical meeting where I’d been instructed to speak only as a patient—not as a researcher—being sick changed people’s expectations of me. Some people would especially doubt my objectivity. They’d reject my ambition to be a leader in a field precisely because I had so much skin in the game. But I knew in my heart that my personal stake in figuring out how this disease worked and how to stop it would actually make me more rigorous in my approach. I wouldn’t stop at a result that was just statistically significant or one that could be published in a medical journal. I would keep going. I would have to. My goal wasn’t tenure, or a big grant, or a medal. My goal was staying alive and saving others with my disease. I would keep validating my findings with experiment after experiment after experiment until I believed my interpretations were true enough to save myself and others. Still, if I revealed my underlying interest in Castleman disease, I thought that my motivation would remain suspect.
And, I can see now, I was indeed naïve. I continued to believe that our relatively small volunteer CDCN team, made up of a few classmates from medical school and a few patients and loved ones, had the needed skills and the necessary bandwidth to accelerate work in a field that had been crawling forward for six decades. We had a lot of work to do to execute our ambitious research agenda and effectively engage hundreds of physicians, researchers, and patients. I did recognize that my new classmates’ skills and knowledge could greatly help us, especially with fundraising and external—outside the CDCN network—communications, which were basically nonexistent. But here again, my fear of being “outed” kept me from recruiting any of them to join the CDCN fight. I was silent on social media. I even deleted old Facebook photos and online articles that mentioned my illness, so that these new business school friends wouldn’t find out about my health. And my trips every three weeks to North Carolina for siltuximab were “to visit family” (which was not untrue). I just worked my tail off in secret and hoped that our outmatched crew could make the necessary progress on our own.
You’d think I would have been smarter about all of this: less proud, less afraid, more realistic. After all, by now, I thought I had a pretty good grasp on hope. I thought I’d seen through some of its pathologies. I’d learned how to activate it, and how to tell the kind of hope that pacifies you from the kind of hope that inspires you to work. But I didn’t see the proverbial light. Hiding my illness may have made tactical sense in one social situation or another, but it put me in a position of siloing my Castleman disease work from the rest of my life.
* * *
—
As much of a misstep as my secrecy was, it bore some kind of imperfect fruit.
I had been meticulously tracking my daily symptoms in a small black notebook. Fatigue: No. Appetite: Good. Enlarged lymph nodes: No. Blood moles: None. And I aggregated data from my weekly blood tests in an Excel spreadsheet. Everything was looking good for me. And now I was also sneaking in visits to the Translational Research Laboratory at Penn in between classes and team projects to analyze the results of blood tests and lymph node studies on my own samples and others and to consume as many medical articles as possible. Alone in my self-imposed silo, I was shocked by what I was finding. It started to dawn on me that the medical community had iMCD all wrong. Not just wrong; the accepted understanding was upside down.
The penny dropped for me one day as I pored over images of lymph nodes from patients with autoimmune diseases, such as lupus and rheumatoid arthritis. The lymph nodes had a set of features almost identical to those taken from people with Castleman disease. In Castleman disease, these enlarged lymph nodes and characteristic abnormalities are considered to represent the initiating factors of the disease and the source of the IL-6. In other words, Castleman disease had always been classified as a “lymph node disorder,” in which the enlarged lymph nodes caused the problems by producing excess IL-6, which then led to hyperactivation of the immune system. From there it was a straight line to organ dysfunction of the liver, kidneys, bone marrow, heart, lungs, and so on.
In lupus, however, enlarged lymph nodes are accepted as a reaction or effect of the disease: The immune system gets hyperactivated, often due to incorrectly recognizing normal tissue as foreign invaders; immune cells proliferate and produce excessive inflammatory signals (including IL-6); and these then lead inevitably to organ dysfunction and sometimes enlarged lymph nodes.
After reviewing the images, I called Arthur Rubenstein to share what I had observed and what I was wondering: Could it be that in iMCD, as in lupus, the enlarged lymph nodes and their unusual features are an outcome of the disease, rather than its cause? Could this be an immune system disorder first and foremost, not a lymph node disorder?
This may seem like a simple distinction. But the order of operations was and is all-important. Misidentifying the symptom for the cause of iMCD could, I reasoned, be the reason its cure remained a mystery. Maybe we were treating it totally wrong—like treating chicken pox with acne medication.
From what I could tell, interpreting the lymph nodes as the problem had become established wisdom through some pretty specious reasoning. Some people were frankly making the case that enlarged lymph nodes must be the origin because all iMCD patients have enlarged lymph nodes with these characteristic changes. But that’s like saying that firefighters must cause all fires because you always find firefighters near fires. We know better.
The firefighting metaphor can be taken further. The lymph node really is like the firehouse of the immune system: It’s where the cells of the immune system go to communicate with one another, train together, and prepare for dispatch. And we know from other immune system conditions that lymph nodes enlarge as a response to immune hyperactivation. Any time of day, and under any circumstances, the cells get the call and assemble in the lymph nodes to coordinate their response.
And the singular focus on IL-6 as the only factor leading to the signs and symptoms experienced by iMCD patients also did not seem to be supported by the data, sparse as they were. Sure, IL-6 was elevated in some patients, and blocking IL-6 helped a portion of patients too—including some with low or normal IL-6 levels—but there were also patients in whom blocking IL-6 did not work. And when IL-6 levels were low or normal in iMCD patients, like me, the results were simply considered to be incorrect. But the coordinated research to develop the panoptic IL-6 test had not revealed any higher IL-6 levels than the traditional tests had. Maybe IL-6 levels didn’t have to be elevated in the blood to be critical to driving the disease in some patients. Or maybe IL-6 wasn’t the problem for everyone and there were other cytokines, which just hadn’t been measured, that were driving the disease in those patients. So, I began to propose that “IL-6” be replaced with “cytokines” in my new model and continued to push forward studies to systematically measure the levels of more cytokines in iMCD patients.
The difference between the old and accepted hypothesis and my new one wasn’t just an interesting intellectual puzzle. It had everything to do with treatment—and
was possibly the reason why none of mine had really worked so far. According to the old model, iMCD should be treated with either chemotherapy to wipe out the cells composing the lymph node tissue or infusions of siltuximab to block IL-6. Well, I was living proof—for the time being—that going after these targets with these treatments wasn’t the right approach for all of us; my iMCD kept coming back.
Instead, and if it all came down to a hyperactive immune system, as I suspected (even if we didn’t know why it was hyperactive), we should be trying so-called immunosuppressants. These are the drugs that people take after receiving liver, kidney, and other organ transplants to stop their immune systems from attacking their potentially lifesaving but foreign new organ. Immunosuppressants weaken the cells of the immune system so they can’t inflict as much damage, for good or for evil, whereas chemotherapy kills everything in its path. And they’re a hell of a lot easier to take than chemotherapy. I was also keenly aware that my current treatment regimen matched the old model, but I wasn’t sad at the prospect of leaving behind the “carpet bomb” mentality of treatment. I was still getting siltuximab every three weeks and chemotherapy every week. It sucked. It’s hard to get more specific than that. Nausea doesn’t inspire eloquence. But I didn’t have any alternatives just yet.
I proposed four possible causes for the immune hyperactivation for future research: a virus (like in HHV-8-associated MCD), a cancerous cell population (like in POEMS-associated MCD), an inherited genetic mutation (as seen in autoinflammatory disorders), and self-reactive B and/or T cells (as seen in autoimmune conditions). I shared my new theory with some colleagues in the CDCN community I was assembling—and didn’t get a particularly encouraging response. I wasn’t necessarily surprised. Even though the CDCN was a novel creation, my colleagues were still all coming to the project with their existing perspectives. Most had years of irreplaceable experience and a traditional introduction to disease research. But, frankly, I was different. I had been well on the way to joining the establishment—but a funny thing happened.
Getting Castleman disease didn’t give my words moral weight. It didn’t make me “more right” about anything. It didn’t turn me into a superhero. What it did was push me off the beaten path—and right into a ditch. From there, things looked a little different.
A part of my ability to bounce back from the agonizingly repetitive Castleman disease attacks was in my focusing on what I was gaining. My disease was terribly peculiar—indeed, that was a part of the problem. But peculiarity has its benefits. In a different context, peculiarity might be mistaken for originality. Originality is the handmaiden of creativity. Silicon Valley has been imploring us to “think outside the box” for decades. If you can get outside the box through peaceful means, or meditation, that’s terrific. But even if you get outside the box via multiple bouts of organ failure, hey, it counts.
I was gaining an ability to see things from an angle—and with an urgency—almost no one else had. I felt this new perspective was starting to pay off, even if select others didn’t yet share my view.
I understood that I now needed to get my hypothesis and supporting information out to the world and that, ironically, I’d have to go the 100 percent traditional route to reach that goal: I needed to publish my proposed conclusions in a hematology journal, the way research has been done for centuries. First, because the best solutions are arrived at only after they’ve undergone intense scrutiny, I knew that I needed to share the data with colleagues who could criticize and poke holes in my logic. I reviewed it with Chris Nabel, my friend who was helping with the CDCN and iMCD research on nights and weekends while taking a hiatus from medical school to get a PhD. He found flaws, we worked together to fix them, and he contributed to the first version of the paper. Now would come the ultimate test: sharing it with Dr. Frits van Rhee.
When I traveled to Little Rock for my next checkup with Frits—as I was now calling him—I brought copies of the papers and data on my laptop that supported this new model for understanding iMCD. He wasn’t surprised to see me parsing through documents and typing on my laptop when he came into the exam room. That was something he’d grown used to. After we got through the history and physical exam, I broke out my notes. I could tell he was choosing his words so as to not knock the wind out of my sails: He was interested, he said, but skeptical.
The next six months involved many conference calls with Chris and Frits after my business school classes, and hours of rewriting drafts, synthesizing findings from the literature, scrapping, and writing some more. We had lots of disagreements; no one held back. This could have been awkward considering Frits had saved my life multiple times and Chris was a good friend. But our disagreements were all in the spirit of getting it right; and we all knew that. After more than a year of steady work and my stabilized health, we were nearly ready to submit the paper for publication. It included an appropriate balance of historical understanding, new possibilities, and future directions. It was bold: We proposed a uniform terminology system for all subtypes of Castleman disease, a new framework for researching and treating iMCD, and hypotheses for the cause of iMCD. This would serve as the foundation upon which all of our future research studies would be based and for the hypotheses that we would test. And the uniform terminology system would serve as the common language that we would all speak. It was a lot and, frankly, ambitious. Arthur Rubenstein (I was still turning to him every week or two for advice) suggested we submit our work to the top hematology journal in the world, Blood. We just had a few more tweaks left to make.
Even though I worried about not being taken seriously as a researcher because of my patient status, I can admit that if I hadn’t been a patient myself with no idea how much longer I had in overtime four, I don’t know if I would have had the brass to propose such a radical shift in thinking at such an early stage in my career. The hierarchical—and often arbitrary—rules of medicine dictate that senior researchers propose these models and synthesize primary data into review articles that summarize the state of thinking, especially review articles in journals like Blood. But having the disease and knowing that I wouldn’t survive without solutions—now—liberated me from this entrenched tradition.
* * *
—
I love medicine. I think all doctors do, even those who get burned out.
I love parsing through available evidence to guide decisions. But Castleman disease made me realize that I love generating data and coming up with solutions more than anything. I was losing patience waiting for other people to generate the data needed to lead to the solutions. I needed new strategies to create more data to lead to more solutions more quickly.
In other words—I was starting to really benefit from my MBA coursework.
It felt great to be back in the classroom, back in the library, back in the books. I was flexing all new learning muscles while digesting case examples of effective collaborations in nonmedical industries, principles of strategic planning, tools for optimizing efficiency, the economics of drug development, and negotiation strategies. I was particularly drawn to the organizational psychologist and Wharton professor Adam Grant’s philosophical model of givers and takers, or the styles that we all bring to our interactions (it occurred to me that there were surprisingly a whole lot of takers in research). And I was inspired by the idea of crowdsourcing through what are known as innovation tournaments. It was impossible to learn about all of these exciting ways to unlock potential and not see how rigid medicine so often was. Even on the research side of things.
It became even clearer to me that the approach in biomedical research of let’s hope the right researcher with the right skill set applies to perform the right study at the right time was backward. Not just because it was inefficient and hopeless—but because I was learning how many alternative ways of doing things there were! There’s no sweeter discovery to someone with a rare illness, I promise you.
Most important
, I was learning that innovation isn’t an art. Innovation, like hope itself, is a force. Innovations are most effectively made with the following systematic approach: inventorying all possible ideas from a wide range of stakeholders, systematically evaluating and prioritizing them, recruiting the very best people in the world, and then working like mad to execute. Sound familiar? In my finance class and others, professors often repeated “hope is not a strategy.” So why, I thought, is it okay in biomedical research, where the stakes are so high?
* * *
—
More than a year had passed since my last relapse, and I continued to keep my health history a secret from my new business school cohorts. But suddenly, I didn’t have a choice. The siltuximab combined with weekly doses of three chemotherapies, which had been part of the cocktail that had induced multiple responses for me, couldn’t keep the iMCD from coming back. Elevated CRP levels, growing blood moles, crashing platelet counts, enlarging lymph nodes in my neck, drenching night sweats. Here Castleman disease was again—for the fifth unbelievable, excruciatingly terrifying time.
This fifth flare also put to rest any lingering suspicion—or hope—that my real problem underlying the iMCD was my liver cancer. There was no way it could be, because it had been removed eight months prior, and an MRI confirmed that the cancer hadn’t come back. It’d only been a comforting scapegoat.
Next to the possibility that I could die was the possibility that—even if I lived—my life would continue to be punctuated by these horrible episodes. Episodes that tore me away from my life, from my work, from my friends, from Caitlin. And that brought me closer to death with each bout. It was agonizing if I stopped to think about it.

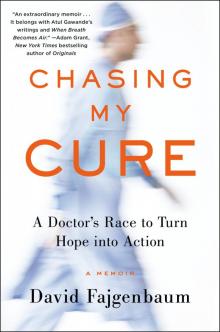 Chasing My Cure
Chasing My Cure